Tissue engineers are exploring the use of minimally invasive bone scaffolds that can act as a template for speedy tissue regeneration, and reduce hospitalization stays and infection risk.
Researchers at The Hong Kong Polytechnic University (PolyU) (PolyU) have designed and fabricated a self-fitting bone scaffold by combining shape-memory foam with hydroxyapatite, the principal mineral component of bone. The scaffold can be implanted into bone defects to induce bone regeneration, enhancing recovery from injuries and fractures.
Despite bone’s regenerative capacity, costly and invasive bone-grafting surgeries are needed to treat large defects caused by tumour removals or severe fractures. Tissue engineers are exploring the use of minimally invasive bone scaffolds that can act as a template for speedy tissue regeneration, and reduce hospitalization stays and infection risk.
A team led by PolyU’s Hu Jinlian, in collaboration with Sichuan University in China, developed a novel scaffold made of shape-memory polyurethane foam—a type of plastic material—and hydroxyapatite nanoparticles. The scaffold is compressed at 0°C and then implanted, eventually expanding to fill in irregular bone defects as it warms to body temperature. Other currently available bone scaffolds do not have such shape-memory, self-fitting properties.
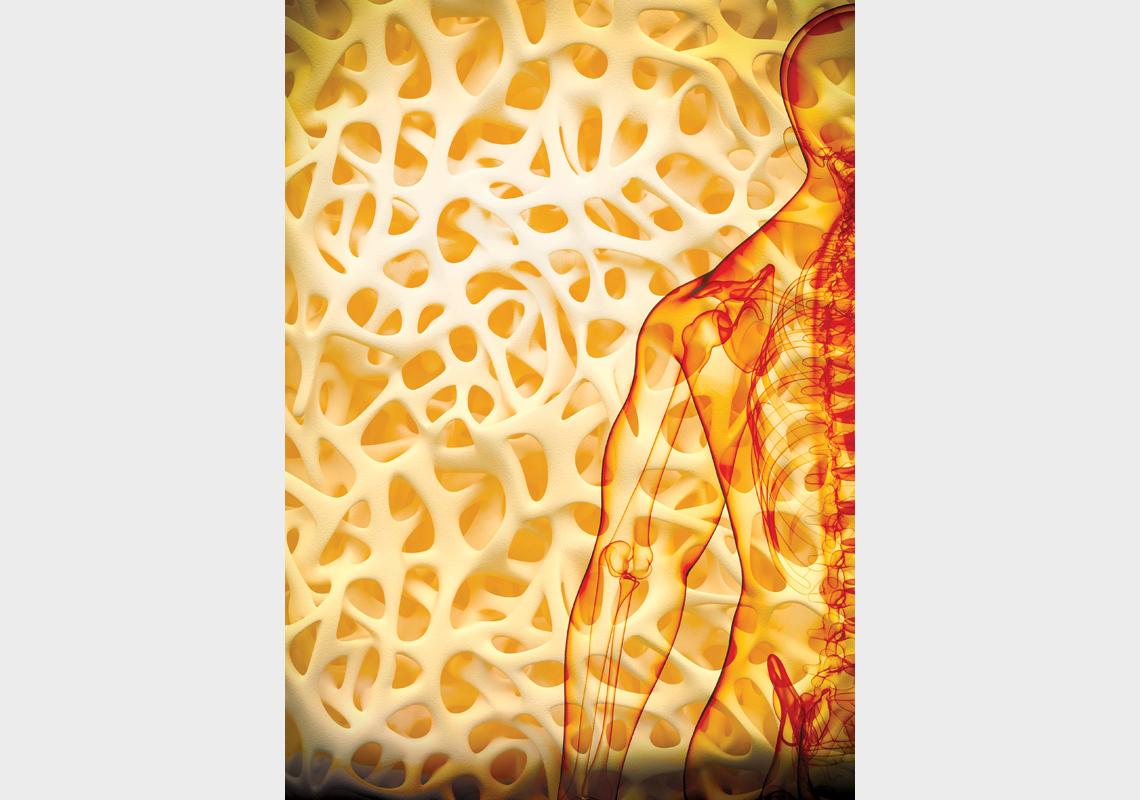
Mimicking the bone’s microenvironment, the scaffold has a highly porous, interconnected structure that allows cells to move within it and generate new tissue. The pores’ sizes and the scaffold’s mechanical strength are similar to those of the inner ‘trabecular’ layer of bone. The scaffold is biocompatible and not toxic to cells.
The team examined how the scaffold facilitated bone regeneration in thighbone defects of nine rabbits, compared to nine rabbits with unfilled thighbone defects. The scaffolds expanded from their compacted shape to fill the bone defects within 60 seconds. Twelve weeks post-surgery, bone tissue had grown into the scaffolds faster than it had grown in the defects in the control group.
Specifically, the scaffold attracted bone-forming cells called osteoblasts and induced blood vessel formation. New blood vessels formed four times faster on the scaffolds than in the control group’s defect areas. Also, 5% of the bone surface was covered by osteoblasts in the experimental group, while almost no osteoblasts were found near the defects in the control group.
“The results show that our scaffold has great potential for bone regeneration. We will work with potential partners to extend the experiments to large animal testing and clinical trials, and will explore more of the scaffold’s functions," says Hu.
For further information, contact:
Professor Hu Jinlian | E-mail: [email protected]
Institute of Textiles and Clothing
The Hong Kong Polytechnic University (PolyU)